Pegasus Knowledge Center

ICD-10 - Opportunity and Challenge
It may seem that the ICD-10 coding changes are a harsh burden on an already stressed healthcare industry; however to some visionaries ICD-10 is an opportunity to improve business practices, increase the granularity of services provided and to improve the quality of patient care.
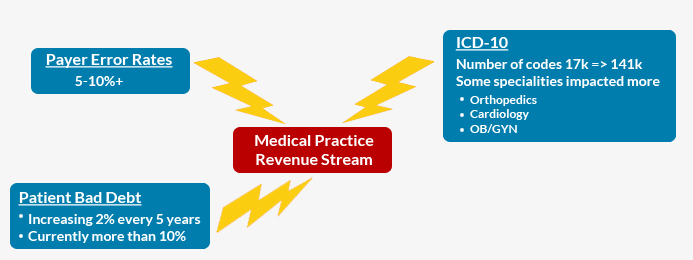
There is no doubt that a large segment of the Healthcare Industry views the mandated changes as onerous and costly, with no corresponding up-side to their individual practices. The second delay in the implementation target date to October 2015 clearly validates industry estimates of 22% of practices have not even started preparation for the ICD-10 implementation. In reality, ICD-10 is just another challenge to add to the already formidable challenges to medical practice financial success. Of all the challenges; however, coding is one of the most frustrating to physicians. They just want to get paid a fair price for the services they have already rendered and coding is just making it difficult for them to collect. The impact of coding complexity also impacts payers. Several of the largest payers have error rates of over 10% and the majority of payers have poor rates of more than 5%. Additionally the high cost of denial processing and the mounting percent of bad debt driven by high deductible policies and increased responsibility of individuals for paying their medical debts are also adding to the downward pressure on practice profitability. Some industry pundits are predicting ICD-10 will cause an increase of between 100 – 200% in denial rates driving Accounts Receivable days to increase by 20 to 40%. With all of these dire predictions it is difficult for some practice managers to see the opportunities.
ICD-10 provides the stimulus and motivation to address some long ignored issues that have dragged down profitability for several years. Industry observers are quick to point out that ICD-10 itself will have the following beneficial impacts on the Healthcare Industry:
- Improve patient care by providing quick access to more detailed information
- Improve the results from clinical research by providing more granular data
- Improve public health reporting and tracking
- Provide more opportunities for innovation (added complexity drives innovation)
- Allows for improved care coordination resulting in improvements in results
- Supports dramatically more accurate and specific detailing of services and procedures rendered, ultimately resulting in improved payment processing.
As the CEO of Pegasus Blue Star Fund, a private equity fund specializing in Healthcare Services Investments, I have over 20 years of experience in investing and managing Healthcare Services companies in the areas of Cancer treatment centers, Surgery centers, Practice management, Medical Group Purchasing Organizations, EHR, Medical Revenue Cycle Management, Patient Portal, Claims Optimization, Claims Authorization, Patient collections, Bad debt collections etc. I am convinced that while there are challenges, the healthcare practices that are managed by visionaries and innovators will seize these opportunities to improve the quality of patient care and dramatically improve the value of their practice. I see opportunities to improve profitability and quality, while decreasing overall long term costs by adopting state of the art technologies such as computer automated coding, integrated EMR and RCM systems, and Medical Business Intelligence Systems. In particular the rapidly evolving technology of Computer Automated Coding provides many benefits to the innovative practices that adopt the technology. Increased coder productivity, potential for increased reimbursement due to more accurate coding, more accurate code assignment resulting in fewer denials, consistency in coding logic resulting in reduced audit risk, and the availability of an easily accessible comprehensive audit trail that supports the quality and auditing functions are some of the benefits derived by using a state of the art Computer Automated Coding system. I would be remiss, if I did not also mention that there are some risks that must be considered and actively managed when using this technology. The initial cost of hardware and software and on-going maintenance may be an inhibitor, however consideration can be given to outsource providers that will provide the coding service based on a usage driven cost structure. Additionally there are several other potential challenges that should be taken into consideration when adopting this technology:
- Industry standards are not adequate to support the automation of all coding
- Providers have different documentation requirements making automation more complex
- EMR systems have Inconsistent formats for their medical records which also adds to the complexity of the automation

In addition to adopting technology to provide automation, error reduction, and quality to the RCM processes; the more innovative RCM providers, such as Orion HealthCorp are working with their clients to help them improve their documentation. Joe Seale, President of Orion, tells us that Orion is aggressively pushing Clinical Documentation Improvement Initiatives (CDII) with their largest clients to help the clients improve their bottom line and prepare for the ICD-10 implementation in a little over a year from now. The clients who have agreed to participate in these initiatives claim that good documentation provides the practice with the following benefits:
- Better clinical decisions based on superior knowledge and insight to the patient's previous treatments.
- Will help ensure that appropriate reimbursement is collected for the care provided
- Improves specificity of measures for quality reporting for each physician
- Supports collaborative care management
- Improves provider profiles for patient care
It is well known that poor documentation, which is so prevalent today, has several negative impacts on a practice:
- Directly affects reimbursement and denial levels
- Reduces the accuracy of quality scores and obscures the significance of observations based on reports that are generated from coded data
- Poor documentation can negatively impact patient care by providing inaccurate or incomplete data leading to incorrect assumptions on the part of the care provider
- Creates exposure to audit risk based on payer questioning the accuracy of the coding of the claims. As more practices seize the opportunity to improve their documentation the overall quality of patient care will improve and industry standardization will become more realistic.







