Pegasus Knowledge Center

ICD-10 - Rethinking the Dual Coding Strategy
Introduction:
For almost two years now the media has been saturated with articles on how best to prepare for the implementation of ICD-10. Over and over we read articles that endorse the dual coding strategy for preparing for the implementation of ICD-10. Theoretically this approach is solid and the best way to go; however realistically this strategy is critically flawed and should be completely re-thought. As the CEO of Pegasus Blue Star Fund, a private equity fund specializing in Healthcare Services Investments, I have over 20 years of experience investing and managing Healthcare Services companies in the areas of Cancer treatment centers, Surgery centers, Practice management, Medical Group Purchasing Organizations, EHR, Medical Revenue Cycle Management, Patient Portal, Claims Optimization, Claims Authorization, Patient collections, Bad debt collections etc. Early in my career I was the CEO and chief business architect for the Pegasus Consulting Group. I had the opportunity to coach the executives from many Fortune 100 businesses in process optimization, and automation, helping them to make dramatic improvements to their bottom lines. My experience over the years has shown conclusively that businesses do not have excess capacity to take on dual entry of data for more than a very short period of time. In fact, when businesses undertake projects that are designed to optimize processes, integrate new technologies, or modify the way business is conducted, they invariably turn to third party providers to assist them with the effort. The assistance varies from temporary staff augmentation to turn key project implementation support; however the primary focus of all of these initiatives is to ensure that current business operations are not negatively impacted during the transition period. Based on my extensive experience on both sides of the project, business owner optimizing operations and third party consultant delivering project support services, and in collaboration with my team of business transformation experts at Pegasus Blue Star Fund I have developed a realistic strategy for transitioning to ICD-10.
Unlike most articles on the topic, we do not pretend to have a one size fits all solution to the ICD-10 implementation. What we do have is a process that any healthcare practice can use to develop the optimal ICD-10 approach for their business. Most importantly, we do not suggest that dual coding is a panacea for implementing ICD-10, it is only a small component of a holistic strategy that addresses all aspects of the ICD-10 implementation mandate.
Holistic Implementation Strategy for ICD-10
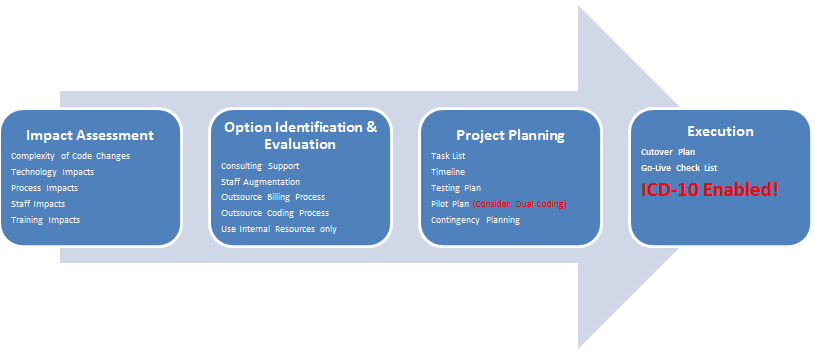
Step One: Impact Assessment
The first step in the process is to determine the magnitude of the impact ICD-10 will have on your practice. This is perhaps the most important step, since unless there is a complete understanding of the impact the changes will have on the business operations, it is not possible to select the optimal solution and the business will either lose or delay reimbursements in the future or equally as bad, expend excessive resources in the form of unnecessary training, technology, or process redesign. Performing the impact assessment can be done by a practice administrator or the practice coding expert by studying the new ICD-10 requirements and then comparing coding and documentation requirements in ICD-10 vs. ICD-9. As an alternative to self-study; consideration can be given for using a third party training provider to ensure that nothing is missed and the practice expert is brought up to speed on the changes quickly. For practices that have outsourced their billing to third party provider a good approach is to request that the RCM company perform the assessment, which they have a vested interest in, since most RCM companies are compensated based on a percentage of the revenue they collect for the practice. The RCM partner will want to ensure that your practice is fully prepared and trained as necessary to meet the new requirements for documentation and coding so that there are no adverse impacts to the revenue stream for your practice or for their business. Another option for the assessment is to retain a consulting firm, which specializes in ICD-10 to perform the assessment for you. Determining the best option for your practice should be based on the skill set of your staff, and the perceived impact on the practice. The most crucial part of the assessment is the timing. Although the implementation has been delayed for another year, the assessment should not be delayed another month. By understanding the impact early, you will give yourself time to develop and execute the optimal solution for your practice, which is the solution that ensures the least negative impact to the business, the greatest positive impact to the business, and is delivered with the lowest cost to the business.
Step Two: Option Identification and Evaluation
As I have noted in previous articles, ICD-10 should be viewed as an opportunity to re-evaluate your business practices and technology. By looking at all available options you may find that solutions you have ignored in the past are now appropriate and necessary in today's business environment. Without a doubt the following key tactical solutions should be considered as part of your ICD-10 implementation strategy:
- Consider outsourcing coding and billing to a third party provider
- Eliminate need for on-going staffing and training issues
- Reduce cost of billing process (normally around 3% reduction based on industry benchmarks)
- Increase reimbursement amount (normally around 5% reduction based on industry benchmarks)
- Reduce AR days
- Implement new technology
- Electronic Health Records (EHR)
- Upgrade billing system
- Patient Portal
- Improve Reporting and Systems Integration
- Implement Business Intelligence Solution (Decision Support and Analytics)
- Automate and Optimize business processes
- Eliminate wasteful or redundant tasks (i.e. duplicate data entry)
- Activate Patient self service via portal
- Scheduling,
- Payments,
- Prescription Renewal Requests,
- Information Requests,
- Etc.
- Create new efficient processes for providers and support staff alike.
Whether your practice will take this opportunity to improve quality of patient care, and improve the practice cost structure or not is completely up to each individual practice and where they are with respect to their competitors. Dale Brinkman, CEO Orion HealthCorp and Jamie Kerestes, Director of Practice Management Consulting for Orion recently performed an assessment on a large medical practice. The report that they provided to the practice is being used to evaluate each option and to develop a strategic plan for moving forward. As you may have guessed the final plan will contain a combination of initiatives, but high on the list is the option of outsourcing the coding and billing function to a third party provider, because the analysis clearly demonstrated that the savings from partnership with an RCM company will result in an overall revenue increase of well over a half a million dollars per year, and a reduction of practice time dealing with staffing and training issues in the coding and billing area. Mr. Brinkman assures me and my staff that these savings are typical of what the rest of the industry is experiencing and that increasing numbers of practices are opting for an outsource solution to their ICD-10 implementation.
As I pointed out in the opening paragraph of this article, many so called, "Industry Experts", are suggesting that dual coding is the right solution for everyone. During the options evaluation process is the appropriate time to look closely at the approach for ensuring that your staff is properly trained in advance of the go-live date. Dual coding can be a partial solution for your practice; however, the full impact must be considered. The following is a list of the impacts that have been mostly ignored by the "experts":
- Most Medical Practices have a small support staff, responsible for many different functions and tasks, of which, coding and billing is only one. This means that there is seldom dedicated staff only responsible for coding.
- The medical practice support staff and professional staff are fully engaged and do not have time to engage in extended training sessions, because there is no one to back them up and revenue is impacted by their absence.
- If a practice decides to duplicate all data entry for a period of time, e.g. 1 month, plans will have to address the cost and training of temporary support staff, or a great deal of overtime will be required of the existing staff.
- A better approach is to evaluate the codes and documentation needed today and compare them with the ICD-10 CM/PCS requirements. Use this information to develop a plan to duplicate only a small, but statistically representative portion of all transactions. Even this approach has a significant impact on staffing.
- Based on the results of the analysis above, a good question to ask yourself is "Can we do a better and more efficient transition by outsourcing our coding and billing?"
- While it is already clear that there is no easy walkway, or automated conversion table for ICD-9 to ICD-10 coding, it is also clear that there are many changes that do not affect every practice. Understanding the impact can help you make the correct decision on the optimal approach for training and implementation. Maybe for your practice the transition is straight forward and all that is needed is a "cheat sheet".
The most important element of this strategy is that every practice must evaluate the magnitude of the impact on their practice and adopt the best solution to meet their needs. My extensive experience with business of all types and sizes strongly suggests that using expert third party support when implementing major changes to processes, products, or practices results in superior outcomes than similar initiatives managed internally. The obvious reason for the improved results is that the third party has experience doing these change initiatives on a regular basis and are aware of the pitfalls, while at the same time they use project accelerators, templates, and expert staff to ensure that the project is managed with minimal impact to the on-going business.
Step Three: Project Planning
Too often the planning phase of the project consists of a quick discussion with the financial team to allocate a certain amount of funds for the project and an equally quick discussion with the providers, coders, and billing staff that amounts to a directive to make sure that you are trained by October 2015. This is really where the rubber meets the road. A true plan must consider the impact of the training process on each aspect of the business. It must ensure there is adequate training, testing, and piloting prior to the implementation day. If new technology is involved the plan must address the implications to the staff, and IT team to ensure that everyone is prepared for the go-live date. Most importantly the practice must be confident that whatever solution they opt for, they will be ready to execute flawlessly in October of 2015. As with all projects there are some key considerations that must be included in the plan. Unfortunately; many organizations seldom undertake a large scale change project and these considerations never hit the radar screen. Project task lists and timelines are often difficult to create because of lack of experience with the possible risks and delays at each step in the project. In general, the timeline must accommodate sufficient time for each of the following steps.
Too often the planning phase of the project consists of a quick discussion with the financial team to allocate a certain amount of funds for the project and an equally quick discussion with the providers, coders, and billing staff that amounts to a directive to make sure that you are trained by October 2015. This is really where the rubber meets the road. A true plan must consider the impact of the training process on each aspect of the business. It must ensure there is adequate training, testing, and piloting prior to the implementation day. If new technology is involved the plan must address the implications to the staff, and IT team to ensure that everyone is prepared for the go-live date. Most importantly the practice must be confident that whatever solution they opt for, they will be ready to execute flawlessly in October of 2015. As with all projects there are some key considerations that must be included in the plan. Unfortunately; many organizations seldom undertake a large scale change project and these considerations never hit the radar screen. Project task lists and timelines are often difficult to create because of lack of experience with the possible risks and delays at each step in the project. In general, the timeline must accommodate sufficient time for each of the following steps.
- Project Orientation: All project participants are briefed on the project mission and goals, the timeline, expectations of their time and quality of their deliverables, etc. The project norms and management structure are also explained at this time.
- Project Execution: If there is technology implementation, or changes required they are completed during this phase. All non-technology tasks are also completed here.
- Project Participant Training,
- Forms and Document modifications
- Desk top and system/process documentation,
- New Reports, Modifications to existing reports, and elimination of obsolete reports.
- Project Testing: During this phase of the project the new technology, processes, documentation, reports, etc. are test thoroughly to ensure that everything is working as designed and the system and processes along with the staff are ready for the new approach for the business. The testing must be coordinated with any third party RCM companies and the Payers to ensure that there are no "holes" in the design and implementation.
- Project Pilot or Parallel: This is the portion of the project when dual coding should take place, however it should be well structured to ensure that the pilot is through and rigorous, but not wasteful and redundant. The pilot should be coordinated with payers and any third party RCM companies to ensure that all aspects of the new processes are functioning as expected and the anticipated efficiencies are delivered. Obviously, if the practice has a partner for revenue cycle management the role of the practice staff becomes quality control and documentation optimization, as opposed to coding and billing execution. A plan that is well coordinated with the Payers will ensure if a payer does have a unique requirement or there are unexpected risks to reimbursements they will be identified in advance and can appropriate modifications to processes and documentation can be made in advance of the October 2015 date.
Note: This is where use of a dual coding approach should be considered. Most production pilots/parallels do include a dual entry type scenario to ensure quality and enhance staff learning and confidence. It is important to carefully control the sample size and content when using a dual entry approach to avoid wasteful redundant activities and include all transaction types based on statistical relevance. - Project Cutover: The project cutover plan must be very detailed so that everyone understands when and how the cutover to the ICD-10 processes and documentation will occur. A good cutover plan will schedule the cutover of as many activities as possible in advance of the actual implementation date. So, for example, providers may start using the new documentation approach in September to provide a month of experience prior to the ICD-10 implementation. This is not dual coding, but select transactions could be used as practice by the coding staff, ensuring a higher quality throughput in October.
- Project Contingency Plan: There should be a contingency plan in place to deal with any project failures or unforeseen contingency to reduce any risk to the business.







